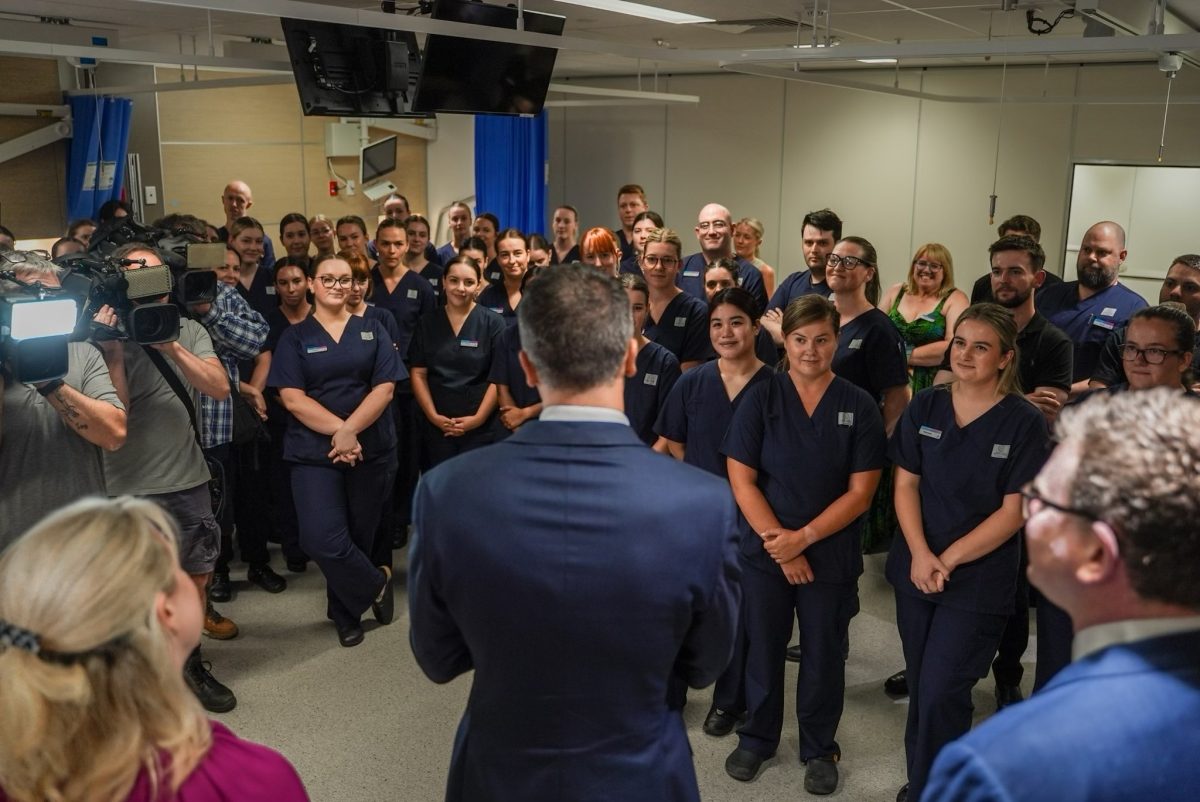
The 314 new graduate nurses will work at sites like the Queen Elizabeth Hospital and Royal Adelaide Hospital across the CALHN. Photo: @PMalinauskasMP.
While the Transition to Professional Practice Program has encouraged the largest intake of nurses to work at the Central Adelaide Local Health Network (CALHN), a recent nationwide survey shows South Australia’s severe shortage of psychiatrists is negatively impacting patient care.
The State Government’s commitment to bolstering its health workforce has seen 832 nurses and midwives employed at public hospitals for the program’s 2024 round, jumping from the standard annual intake of around 600 nurses.
South Australia Minister for Health and Wellbeing Chris Picton said they’d be instrumental in boosting nurse numbers to service the 150 inpatient beds opening this year at the Queen Elizabeth Hospital, Flinders Medical Centre, the Repat and Lyell McEwin Hospital.
Although the 12-month placements with further education and on-the-job training have seen a total of 206 nurses and midwives employed across six regional LHNs, there’s still concern about mental health resources, especially outside the cities.
Last year a report submitted to the State Government found that mental health resources in regional areas were so poor, that higher numbers of psychiatrists per person could be found in Mongolia, Ukraine and Russia.
This is in contrast to Adelaide’s metro area, which has the highest ratio in Australia.
According to the report, the current situation came about due to the failure of successive governments to appreciate rural mental health challenges and take responsibility to drive mental health service enhancements.
University of Western Australia Associate Professor Mathew Coleman, an author of the report, said the lack of country representation in the state’s health bureaucracy and funding competition with Adelaide’s LHNs were discriminatory and unjust.
“There’s a lack of accessibility of services; there’s long wait times; they have to travel inordinate distances to be seen – or not in many respects – and the people at the coalface, the clinicians in country South Australia doing their darnedest, eventually become demoralised and dejected,” Dr Coleman said on The World Today.
He also noted the existence of a Minister for Regional Roads, but not one for mental or rural health.
In a recent survey of 1269 psychiatrists across the country, the Royal Australian and New Zealand College of Psychiatrists (RANZCP) found that mounting pressures on the SA workforce saw 69 per cent of respondents experiencing multiple syptoms of burnout in the past three years.
The survey also illustrated that close to 40 per cent of SA psychiatrists were considering an exit from the profession in the coming five years, second only to Western Australia.
Chair of the RANZCP’s SA branch, Dr Patrick Clarke, said the survey findings underscored the severity of the workforce shortage crisis in the state’s mental health system.
To amend the situation, Dr Clarke said the Commonwealth and State Government needed to collaborate with targeted and sustainable investment in the SA psychiatry workforce to ensure that mental health facilities were adequately resourced.









