Danielle Mazza* discusses what needs to change it improve access to sexual reproductive health services.
 When the American legal precedent protecting women’s right to an abortion in the United States, Roe versus Wade, was overturned last year, women around the world felt anxious.
When the American legal precedent protecting women’s right to an abortion in the United States, Roe versus Wade, was overturned last year, women around the world felt anxious.
In Australia, despite abortion being legal, there was increasing concern about women’s ability to access abortion.
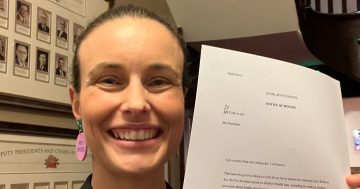
This led to a Senate inquiry into universal access to reproductive health care.
This inquiry has now concluded. A key recommendation is that:
all public hospitals within Australia […] provide surgical pregnancy terminations, or timely and affordable pathways to other local providers.
This recommendation has been welcomed by abortion advocates around the country.
But why is a recommendation like this necessary? Why don’t hospitals already provide abortions?
A safe, common procedure
Abortion is a safe, routine procedure that nearly one in five Australian women who have ever been pregnant will undergo by the age of 45.
Abortions can be provided either medically or surgically.
A medical abortion is a medically induced miscarriage.
In Australia, the medication needed to have an abortion is registered for use until a woman is nine weeks’ pregnant.
Many women prefer a medical abortion as the medication can be taken and the abortion occurs in the woman’s own home.
But a medical abortion is not for everyone.
Some women may not be able to manage it at home, don’t have a safe and private space, or have health issues that preclude a medical abortion.
Some women miss the nine-week cut-off for a medical abortion because they don’t realise they are pregnant, or they make the decision to abort after nine weeks (this sometimes happens because of a relationship breakdown when the woman finds out she is pregnant), or because of other issues such as domestic violence, rape, drug use or mental health issues.
Surgical abortions usually involve a woman having a suction curette to remove pregnancy related tissue from the uterus under sedation in a hospital or day surgery centre.
Some women prefer this approach as it’s quicker.
A surgical abortion also gives women the opportunity to have an intrauterine device (IUD) inserted for future contraception.
It’s important for women to have a choice about the type of abortion they have and for surgical abortion to be also be available for women who find out later in the pregnancy there is a serious problem with the fetus.
So why is access so patchy?
Many hospitals, particularly those outside major metropolitan areas, don’t currently provide any abortions, let alone surgical ones.
Our research has found many hospitals discourage referrals from general practitioners.
There have also been reports of hospitals turning away women who need care in the uncommon event of complications following a medical abortion.
The reasons for this are complex.
Abortion remains very stigmatised in our community.
Few gynaecologists want to perform the procedure.
Training on how to provide abortion has not been a routine part of gynaecology or GP training and there is a shortage of trained providers, particularly for complex cases.
Hospitals haven’t felt obligated to provide abortions.
To date, no-one has held them accountable for providing this essential service.
There has also not been any regional-level planning to ensure services are locally available.
Some health professionals are also conscientious objectors who believe they should not be forced to provide abortions.
What does it mean for women needing an abortion?
As the Senate inquiry report states, it’s a postcode lottery.
Many women don’t know how to get an abortion, what’s available or where to go.
Some will look online or go to their GP.
If they decide on a surgical abortion, their local public hospital may not offer this and so their only option is a private clinic.
Many of these clinics have closed in recent years and more are open very limited hours or staffed by fly-in-fly-out teams, which means they can be very difficult to access.
Women may need to travel long distances to get a surgical abortion.
This means taking time off work, organising childcare (as many women who have an abortion already have children and arranging accommodation.
This all comes with significant out-of-pocket costs.
How can we fix the system?
The Senate inquiry recognises many public hospitals, particularly women’s hospitals, that receive public funding are faith-based and will not allow abortions to be delivered at their premises, even if the doctors and nurses want to offer them.
The inquiry’s key recommendation seeks to ensure all public hospitals provide surgical abortions – and if not, at least ensure women in their catchment can access timely and affordable care via other local providers.
The inquiry also recommends that contraception and abortion access (particularly for rural and regional women) is made available via publicly funded community and hospital-based services, with regional-level planning, training and accountability.
To make this a reality, there has to be consequences if it doesn’t happen.
Funding should be tied to provision.
For full transparency, hospitals should also be made to issue public reports that spell out how many and what type of abortions they provide each year.
Funding also needs to be offered to train health professionals to deliver the services to ensure that now and into the future, we have a health workforce capable of delivering the services needed.
GPs need to know that if they provide a medical abortion, their local public hospital will provide support and see patients if and when needed.
GPs also need to have clear referral pathways so women can get into surgical abortion services in a streamlined and timely way.
Finally, women need assistance to navigate to abortion services when they need to.
The inquiry recommends governments develop coordinated campaigns and education materials to improve women’s knowledge of their rights and options for accessing effective contraception and abortion care.
It also recommends establishing a national information services like the Victorian 1800myoptions hotline.
While the recommendations are a step in the right direction, action is needed to translate these recommendations into actual services on the ground.
The government’s response is eagerly awaited.
*Danielle Mazza, Director, SPHERE NHMRC Centre of Research Excellence in Women’s Sexual and Reproductive Health in Primary Care and Professor and Head of the Department of General Practice, Monash University
This article first appeared at theconversation.com