Southern NSW Local Health District (SNSWLHD) CEO Margaret Bennett, Member for Bega Dr Michael Holland, and SNSWLHD general manager Brad Scotcher at the Eurobodalla Health Update on 7 November. Photo: Marion Williams.
The latest update on the new Eurobodalla Regional Hospital was encouraging and included discussion about a local radiotherapy service.
Southern NSW Local Health District (SNSWLHD) CEO Margaret Bennett, general manager of coastal network Brad Scotcher, and Matthew Malone, project director of health infrastructure, along with Member for Bega Dr Michael Holland, spoke and answered questions, both previously submitted and from the floor at Moruya Golf Club on Thursday, 7 November.
They assured people that the new hospital, due for completion in 2027, would operate as a level four hospital from day one. They said there was ample room to expand the hospital’s facilities as the shire’s population grew, and Ms Bennett expressed confidence around attracting the workforce needed.
The big news was that work is underway on an expressions of interest (EOI) document for a local radiotherapy service (LRS) for the hospital. It is a service that a group of people have been passionately advocating for the Far South Coast’s ageing population so they don’t have to travel to Nowra, Canberra or Sydney for the potentially lifesaving treatment.
Ms Bennett said they had been working with the Federal and NSW governments. “The minister is working with us to develop an EOI to test the market and gauge interest for providing radiotherapy.”
She said the EOI document would include a range of options and hoped it would be out early in the new year. The EOI would give the government an idea of the cost of the LRS, as well as models and ways to go forward.
“It is a market test,” Ms Bennett said. “It isn’t a green light,” adding she wanted to see the new hospital open with a stroke unit, fully staffed intensive care unit (ICU) and accommodation for nurses.

Southern NSW Local Health District CEO Margaret Bennett speaking at the Eurobodalla Health Update on 7 November. Photo: Marion Williams.
She said staffing the hospital was a big focus and SNSWLHD was working with the minister on the “financial uplift” needed.
“We have a plan of what we need and when we need it,” Ms Bennett said. “My confidence is growing, but in an environment where there is a national challenge with nurses, medical and allied health staff.”
SNSWLHD has successfully recruited staff from overseas and has partnerships with three universities, in Wollongong and Canberra, to grow its junior medical workforce.
“The hospital will open with a simulation centre which is a great training facility,” Ms Bennett said. “It enables us to have undergraduates for longer so they are more likely to stay.”
She is hopeful of an announcement of funding for nurses’ accommodation and that the Eurobodalla may be one of the sites selected.
In preparation for the ICU, Moruya Hospital now has a close observation unit. In a video, Dr Luke Mitchell, the close observation unit clinical lead at Moruya Hospital, said the ICU would attract more specialists to the area.
Mr Malone said the hospital site was 22 hectares so there was ample room to expand it as the population increased.
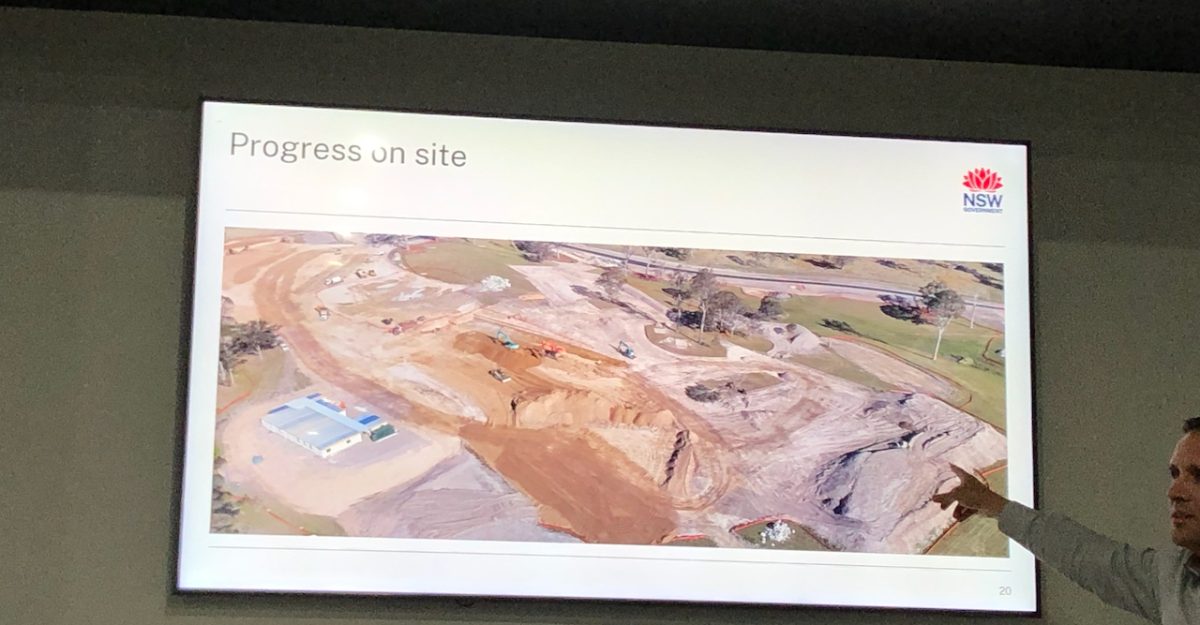
Southern NSW Local Health District’s project director of health infrastructure Matt Malone showed the audience an aerial shot of the hospital construction site, showing progress. Photo: Marion Williams.
He said the hospital’s floor size was twice that of the Batemans Bay and Moruya hospitals combined.
When asked how many beds the hospital would have, Mr Scotcher said there would be capacity to have more beds in every service, but modern hospital service delivery didn’t revolve around the number of beds. People could be treated in procedure rooms and bays, and there was greater focus on ‘hospital at home’ than previously.
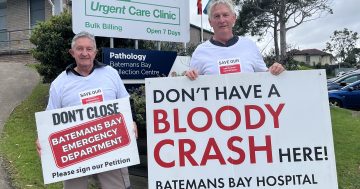
Batemans Bay residents continued to express concern about the loss of the Batemans Bay emergency department when the new hospital opened.
One man spoke about the travel time from Batemans Bay to Moruya in a medical emergency in the absence of a bypass, reported a 45-minute wait for an ambulance, and said he was turned away from the urgent care department on a Saturday and told to return on Monday.
Ms Bennett and Dr Holland are looking at what they can do to increase the urgent care department’s opening hours and it may be open 12 hours a day in December.
Mr Malone said the completion time for the new Batemans Bay Community Health Centre will be confirmed when the contract is awarded next year.
Dr Holland said he had not supported the 18,000-signature petition to keep the Batemans Bay emergency department open because it would have prevented the shire from having a level four hospital. “Lives are being risked by not having a level four hospital in the Eurobodalla,” he said.
“Closing the gap in health outcomes is what we have to do in the Eurobodalla, not only in terms of Indigenous healthcare, but also the inequity compared with other areas,” Dr Holland said. “To have a level four ICU means everything else goes up to level four.
“The whole principle is to improve general care,” he said.
Original Article published by Marion Williams on About Regional.